It is National Health Center Week! Between August 8 and 14, advocates of the federal health center program from across the country have hosted events and are getting the message out about the extraordinary work community health centers accomplish within the communities they serve.
The theme of National Health Center Week (NHCW) this year is, “The Chemistry for Strong Communities.” You can head over to the NHCW website if you’re interested in learning more about the Community Health Center program through the lens of this year’s theme.
We, at Atrómitos, are long-standing supporters of the Community Health Center program. We have worked in, alongside, and in support of Federally Qualified Health Centers (FQHCs) and FQHC lookalikes. We understand the critical role the program plays for the many patients who receive care within Community Health Centers.
We also firmly believe there are lessons on efficiency, innovation, and compassion that large swaths of the healthcare infrastructure can learn from Community Health Centers across the country. (For our data-driven readers, see the Community Health Center Chartbook 2021 from the National Association of Community Health Centers.)
In short: we believe Community Health Centers are great. But we recognize that not all of our partners may know much — or anything — about these vital providers in our country’s healthcare safety net infrastructure. So this week, in celebration of #NHCW2021, we want to share with you an idea about health centers and the Community Health Center program in hopes that you may learn something new, be reminded of something you forgot, and participate in advocacy supporting health centers whenever you get the chance.
Community Health Centers are universal healthcare
The United States has been trying to figure out how to best provide healthcare to its citizens and residents for years. And while the previous hyperlink only goes up until the passage of the Patient Protection and Affordable Care Act in 2010, we all know the debate has continued on since then.
Some of us may remember this graphic from WaPo where each of the (initially many) 2020 Democratic presidential candidates stood regarding a Medicare-for-all approach to healthcare.
When the country isn’t debating what to do next with healthcare, it is trying to decide if what we are currently doing is enough, or even legal. (My colleague, Tina Simpson, has spent many articles talking about the legal challenges that have faced our current federal healthcare law, but here’s the most recent one.)
The point? Healthcare is one of those seemingly unanswerable questions facing the United States.
Except, in some ways, it is answerable: Community Health Centers.
One of the ideas behind universal healthcare, according to the World Health Organization (WHO), is that “all people have access to the health services they need…without financial hardship.” Per Section 330 of the Public Health Service Act, which authorizes the existence of and governs the Community Health Center program, patients of community health centers cannot “be denied health care services due to an individual’s inability to pay.”
If you were to walk into a community health center today and be financially unable to pay for any service you requested, you would not only be provided the service requested (assuming, of course, said service was provided in the health center), but staff would also work to identify any other preventive or treatment service you may need to maintain or improve your health status. By design, a community health center is required to provide an access point to healthcare services for anyone.
Another component of universal healthcare, also per the WHO, is that “should be based on strong, people-centered primary health care.” In addition following guidelines on where they operate, who they offer services to, and how those services are provided, community health centers must also follow mandates on how they are governed. Revisiting Section 330 of the Public Health Services Act, one learns that health centers are to establish “a governing board which…is composed of individuals, a majority of whom are being served by the center and who, as a group, represent the individuals being served by the center.”
What does this mean?
It means the body responsible for making decisions on how a community health center provides care is doing so through the viewpoint of the actual patients receiving the care. When community health centers face their Operational Site visits to prove to the Bureau of Primary Health Care (the component of the United States government responsible for monitoring compliance of the Community Health Center Program) that they are following all of the Section 330 regulations, one of the requirements they must meet is having a Board of Directions where at least 51% of members are patients. This patient-driven governance helps leadership within the community health center deliver services that are identified as necessary by patients and are offered with the patient experience at front of mind.
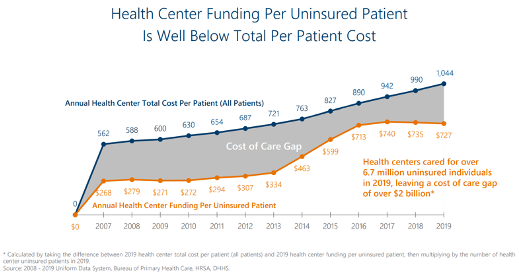
Is offering services regardless of a patient’s ability to pay an easy financial sustainability plan to enact? No, as is demonstrated by Chart 1, below.
Are all community health centers easily able to populate a Board of Directors while maintaining a 51% membership of patients? No. (And while we have talked to you in the past about Board diversification, we did not tackle the concept of patients-as-Board-members.)
But community health centers work to accomplish these things anyway, because they believe in the right of all to have access to healthcare that provides them the services they need.
Some concluding thoughts
If you aren’t sold on the Community-Health-Centers-as-Universal-Healthcare concept, that’s OK. As we said earlier, the universal healthcare conversation is here to stay in the United States for at least a few more years.
However, we do want you to walk away from this post with continued, newly found — or re-identified —appreciation for the Community Health Center Program. If you have not yet reviewed the afore-linked Community Health Center Chartbook 2021, here’s a couple of TL;DR stats:
- Community Health Centers provide care to 1 in 11 people in the United States
- Individuals who are uninsured or publicly insured comprise 81% of Community Health Center patients
- Between 2009 and 2019, Community Health Centers increased their employed Clinical Staff (in FTE) by 116%
- Patients at Community Health Centers are less likely to report unmet or delayed access to care when compared to both other clinics and private physicians
There are countless other statistics and volumes of other information we could provide you on the benefits of community health centers and how they are incredible stewards of the public dollar. The Community Health Center Program, in our eyes, does not always get the recognition it deserves.
So during this year’s National Health Center Week, we hope you take a moment of your time to learn about, recognize, and support community health centers.
